Maxillary and orbital trauma in children—why you should invest more time in these surgeries
BY DR DAMIR MATIC
The treatment of pediatric maxillary and orbital trauma is really a passion of mine, and a focus of my practice in Canada. For children with trauma, the important difference is that they’re still growing. That means we always worry about their growth after reconstruction is finished and follow up is extremely important. In reviewing surgical approaches to pediatric trauma, it’s useful to first consider how the face grows. How can we use this knowledge to better treat our patients?
What is clear in the literature is that facial growth is really genetically driven. That’s why you look like your parents and your children are going to look like you. A lot of the time that’s out of our hands. The amount of epigenetic influence is quite minimal.
Of course, there are no growth centers within facial bones, and the bones of the face grow by deposition resorption and by suture separation. Really early on, the primary driver of facial growth is brain growth. As that brain develops and as your brain expands, it pushes the face out and down. It really determines how large your orbits are and how wide your face is.
Epigenetics do have a role, but it’s probably less than 10% to 20% of facial growth. This involves muscle action, primarily the bigger muscles in your face, like the muscles of mastication. The face also expands as the sinuses develop, and when adult teeth erupt the maxilla and mandible grow vertically in height.
When we look at the pediatric facial skeleton, it's different to the adult skeleton. The pediatric skeleton is primarily cranium, with a small facial volume. It's an 8:1 ratio compared to 2:1 in adults. We’re born without sinuses then start developing them: the maxillary sinus around five to six years of age, and the frontal sinuses again around six to eight. Then, tooth eruption happens around six to eight, which guides vertical growth of our mandible and maxilla. By seven to eight years of age, our cranium and our orbits are about 80% to 90% of the adult size, so an injury at that stage is going to cause less growth disturbance than an injury at six months of age, before things have developed.
The remodeling potential of the upper face versus the mandible
In reviewing the trauma literature, it’s clear that the earlier the injury happens and the higher the energy of the injury, the more growth disturbance there’s going to be. This growth disturbance will occur despite our treatment. If a child gets injured at two years of age, there is going to be a more significant impact on growth compared to an injury that occurs at eight or nine years of age.
The other issue here is that the upper face is pretty much static. There are very few forces acting on the upper face other than the brain growing, potentially the septum pushing and some of the mastication muscles pushing the upper face. There’s really no function or movement beyond that. As a result, the upper face has a very low opportunity to remodel after an injury, compared to the mandible. As a stress-bearing bone, the mandible is constantly moving and has larger muscles acting on it, so it can remodel significantly better than the orbits and the maxilla. If we're not anatomically perfect on the mandible, there is a good chance it will continue to improve, based on the forces applied by soft tissue and muscle action. The same is not true in the orbits and maxilla—that's very clear in the literature.
So, the general factors that affect growth are obviously the nature of the trauma, the age at which that trauma happens—so the earlier it happens, the worse the potential growth disturbance—and finally, surgery itself can potentially affect growth by leaving a scar or manipulating the soft tissue and bone. Lifting the periosteum is potentially detrimental, and so is putting hardware across bones or across sutures.
The literature is less clear on the type of hardware, but we certainly know that if you’re keeping the hardware for a long period of time, that’s not as good as having hardware that potentially resorbs or isn’t there. If the child's not allowed or cannot function, this is more detrimental to the mandible because now the mandible can't remodel. Those are all the main factors that come into play during a trauma.
Turning now to the orbits and maxilla, adult size is reached at least in anterior growth projection by age eight. After age eight, as the adult teeth erupt, the maxilla will continue to grow vertically, but anterior growth is not happening to a significant degree. The children that we see who are at the highest risk of this injury are those who have just started to become mobile, so from around age four to eight.
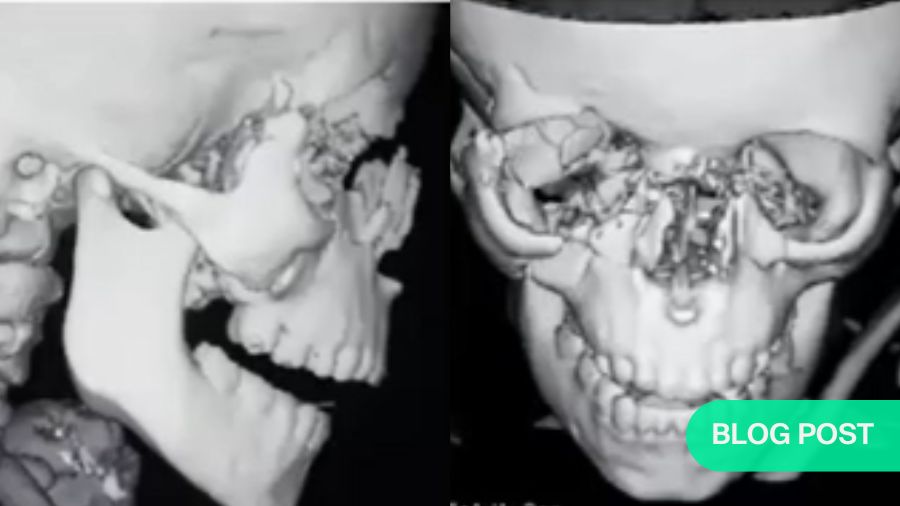
The orbits and maxilla have very little remodeling ability, so that means they're not going to change after the trauma. That also means they're not going to change after our surgery. If we're going to get this right, we must get precise anatomic reduction of these bones to give them a chance to grow normally.
The best patient series that I am aware of belonged to Joe Gross, who presented about 18 cases in children from four to eight years of age when they had their injury. They had pan-facial fractures and he followed them for over 10 years. His series clearly showed that the children who had the best anatomic reduction at the time of trauma repair, particularly of the midface and orbits, grew the best and needed fewer surgeries down the line when they were adults.
In short, the better we put those bones together, the better these children grow and the more normal they appear at the end of growth.
Understanding the unique nature of pediatric facial trauma
The nature of the trauma also plays a major role. Low energy injuries tend to be sporting injuries or falls. Thankfully, these types of trauma tend to give you large fracture fragments. These can be treated through a minimally invasive approach; and often don't need hardware. They may require a closed reduction where we lift the bone into position, but the soft tissue helps us. The periosteum is thick and holds the bone in position, so you can often get away without putting hardware in these children. Obviously, if the bone is not stable you might have to add minimal hardware, or a wire, just to hold it in position, but that’s all.
In high energy injuries, with bones in small pieces and displaced and where the soft tissue is hurt, cut, and bruised, that's where we must have precise anatomic reduction and rigid fixation to allow the bones to heal in position.
The injuries that happen that are low velocity tend to be in the upper face, because these are bigger parts of the face. In terms of the midface, we're talking about the zygomatic arch, the zygoma, maybe the NOE or the nose primarily. They tend to be greenstick injuries. The bones are more cancellous than cortical, so the bone is softer, more "rubbery". The fragments are large and there's less comminution. Again, the displacement is limited, and they tend to be isolated injuries.
Orbital wall fractures are quite unique, pattern-wise, in children compared to adults. We see two separate types of injuries that are less common in adults. The first is an orbital roof fracture, because young children don’t have a frontal sinus which starts developing at age eight.
If the frontal sinus is not present then it can’t act as an airbag, so it doesn’t really protect the brain or the roof of the orbit. The trauma therefore hits the superior orbital rim or frontal bone and causes a fracture along the roof and injury to the central nervous system too. The fragments don’t go into the brain; the brain pushes them down into the orbit. When they’re in the orbit, they cause a reduction of volume. These types of injuries tend to happen in slightly younger children, when the head is a bit smaller compared to the face. They come with CNS injuries and often need to be treated not only by us but together with our neurosurgery colleagues.
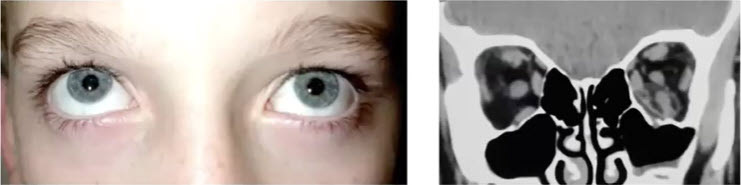
Roof fractures are often blow-in type fractures in which the bone fragments push down into the orbit. The patient will present with proptosis—the eye will be down and out—they might have double vision and sometimes significant pressure on their globe, so we often want our ophthalmology colleagues involved as well.
Roof fractures can be significant issues, so when you're in the emergency room you want to check if the patient has double vision, if they can move their eye, if they have ptosis, if they have mydriasis. These are important things to rule out.
The importance of fast emergency responses and meticulous surgical techniques
Now, let's look at orbital floor fractures. These fractures tend to occur in slightly older children when the maxillary sinus develops, and it’s where we see the most serious problem in the eye. The Trapdoor fracture—or white-eye blowout as we call it—is a pediatric problem, and it’s extremely rare in adults. The patient will often present with no bruising or swelling. They look fine except they may have nausea and vomiting. However, they will have pain if they move their eye, and sometimes they don’t want to open their eyes because it hurts, so they’re squinting. This unique pediatric injury involves the squeezing of the inferior rectus muscle in the fracture site. That muscle, if not released, will undergo necrosis and the patient will have diplopia for the rest of their life, so this is an emergency. They might present squinting, or they cannot look up when asked—which is a big concern. The key is to take them emergently to the operating room in order to release the trapdoor, enlarge the fracture and free up the inferior rectus muscle.
Can implants help here? The literature relating to implants in the orbit is unclear. People tend to feel uncomfortable putting artificial alloplastic material in very young children—say under four—so experts would suggest autogenous material like bone or even cartilage. Sometimes no implant is necessary if we are talking about a small fracture. If the child is over eight, the orbits are near adult size, so using titanium or other materials is appropriate because the orbit isn’t growing anymore. This decision depends on the comfort level of the surgeon. It’s always safer to use autologous material in very young children, but I would suggest that after eight you can use any material. Then, the surgical approach to the floor through the lower lid is based on surgeon experience and preference which is similar to adult surgery.
My takeaway message for successful outcomes is to spend more time doing these surgeries. I approach the surgery, reconstruction, and closure of the skin and mucosa more meticulously, because children's scars tend to be more aggressive, can affect growth, and ultimately outcomes which may lead to more surgical procedures.
Video: AO CMF Expert Case Discussion—Managing Primary and Secondary Pediatric Midfacial Trauma
Damir Matic, Mohamed Abdulazeem, Mohamed Amin, Amr Amin Ghanem and Amir Elbarbary are presenting webinar about management of primary and secondary pediatric midfacial trauma.
About the author
You might also be interested in:
AO CMF Global Study Club
A reliable and dynamic platform where AO CMF members can get together locally to discuss compelling cases, exchange experiences, and network.
Clinical library and tools
Explore our educational resources for materials designed to develop your competencies and improve your patient care.
My Biggest Challenge
Damir Matic discusses his most difficult clinical case and how he managed it.
Surgery as an artform
Damir Matic talks to AO about his passion for art and shares some of his work.